When my son Charles was nine, I found a collection of candy wrappers under his bed and I cried. Substance use disorder ran on both sides of the family, and I knew that his stash of sweets meant he had a sugar addiction. I was determined I could prevent a future drug addiction. Trouble was, I had no information on which to base a strategy.
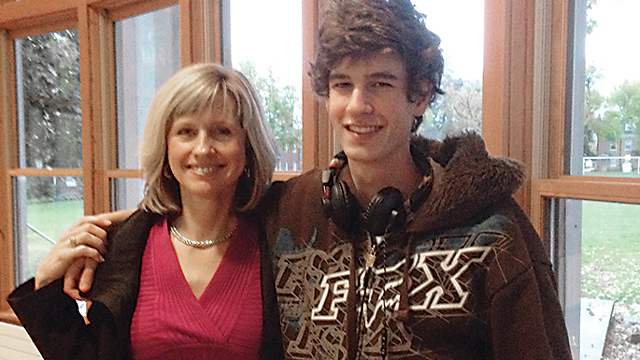
Charles was an enormously popular kid – funny, thoughtful, as well as a lyrical and creative genius. The personality trait that worried me was his relentless pursuit of fun.
I remember a trip we took to King’s Dominion when Charles was twelve. Once we got home from this all-day outing, he asked if we could go to Busch Gardens. He meant right then.
I laughed and said we’d have to plan for another day. So he shifted tactics and begged to have four friends come over for dinner and a sleepover. When I said no, he asked if we could have just two over for dinner, which would likely turn into him pleading for them to stay overnight. I knew he’d then keep them up all night long playing games.
I would later find out this relentless pursuit of fun was the result of a broken reward system, a concept that was introduced to me in a lecture by Kevin McCauley, MD, who is an expert on the brain science behind addictive behavior. Even later, I would discover this behavior could be labeled “sensation seeking.”
Unfortunately, over the years, I was unable to prevent his addiction and despite my best efforts, Charles took his own life at age twenty while experiencing an episode of major depression and withdrawal from heroin.
Preventing the kind of devastating addiction Charles experienced starts with a proactive approach to understanding mental illness, brain science, and the inherited personality traits that drive drug addiction. For too long, we have swept these issues under the rug, not recognizing them as disorders of the brain, but labeling them instead as lifestyle choices or moral failings.
We now have the opportunity to embrace an evidence-based solution for preventing drug abuse and addiction in adolescents by targeting inherited risky traits before they cause problems.
The program is called Preventure. A school-based prevention intervention program recently featured in The New York Times, Preventure was identified in the Surgeon General’s Report as an evidence-based addiction prevention strategy associated with up to 80 percent reductions in alcohol and drug use in program participants at the 2-year follow-up point.
Instead of fear-based programs, Preventure focuses on teaching at-risk teens the life skills to manage one of the four personality traits that put them at risk for addiction: sensation seeking, impulsiveness, anxiety sensitivity, and hopelessness. Three of these four behaviors are also red flags for mental illness.
Jasmin Vassileva, PhD, is an associate professor of psychiatry and psychology at VCU, and the only mental health professional in the United States at this time seeking to implement the program. Dr. Vassileva and Preventure developer Patricia Conrad, PhD, a professor of psychiatry at the University of Montreal, have worked together for more than twenty-five years. The pair plans to seek federal funding to test Preventure at Virginia high schools in the 2017 school year.
“Despite being included in the Surgeon General’s Report on addiction, Preventure has not yet been tested in the United States,” Dr. Vassileva said, adding that it has been implemented successfully in other countries including Canada, Australia, and the Netherlands. “Our goal is to make Virginia the first U.S. state to pilot the intervention program.”
To identify teens who might benefit from the intervention, all students at a school are given a 24-question personality screening at the start of the school year. Months later, two 90-minute courses on how to best channel your personality for success are offered, and most students sign up.
The students who score high on a particular trait are slotted into the courses specifically tailored to help them address their most troublesome trait. These training sessions are taught by Dr. Vassileva’s staff, or teachers or other counselors can be trained to deliver the courses to students, depending on the resources available at the school. According to Dr. Vassileva, about 45 percent of the kids end up taking one of the courses.
In order to qualify for the trial and apply for the grant at the National Institutes of Health, Dr. Vassileva has to have commitment from at least thirty schools or institutions.
At press time, enrollment had begun, and there may still be openings. For more information, contact Dr. Vassileva at jasmin.vassileva@vcuhealth.org or call 804-828-5807.
While this initial scope might focus more on schools, the life-skills training could be adapted in other settings to benefit those already suffering with a substance use disorder.
As a mother who lost a son to addiction and concurrent mental illness, I encourage you to let educators and physicians know we are willing to embrace innovative programs like Preventure in Virginia’s schools. Silence and denial have been detrimental to implementing solutions for an epidemic that is getting worse. It’s time to recognize it as a brain disease and talk openly about it.
![]()