When Delano Dulin got sick in June of 2021, his parents assumed that it was a bout of COVID or some other kind of virus. Until that time, he was a normal and healthy fourteen-year-old boy who enjoyed playing video games. Delano’s mom Jessica says her son looked horrible.
After multiple trips to the local urgent care, where doctors repeatedly said it was a virus, Delano, who lives in Richmond County in the Northern Neck with his family, wasn’t getting any better. Jessica started to feel her instinctive mom senses activating.
“He looked like the walking dead. He had a rash that was spreading and he started getting ulcers in his mouth. He lost twenty pounds in a week. I knew something was very wrong,” says Jessica. Things took a turn for the worse when Delano started urinating blood. That’s when his mom had had enough. “I called his pediatrician,” says Jessica, “and she said, ‘Stop whatever you’re doing and take him to the emergency room.’” When they arrived at the ER, Jessica says Delano was quickly hooked up to an IV and a catheter was inserted. “Within forty-five minutes, we were on our way to VCU.”
Delano stayed in the critical care unit at the Children’s Hospital of Richmond at VCU for two weeks and during that time, he was diagnosed with an extremely rare disease called granulomatosis with polyangiitis. Formerly called Wegener’s, the disease affects about three out of every 100,000 people and restricts blood flow to organs and tissues, sometimes causing permanent damage. The cause of the disease is unknown, and it can be fatal if left untreated.
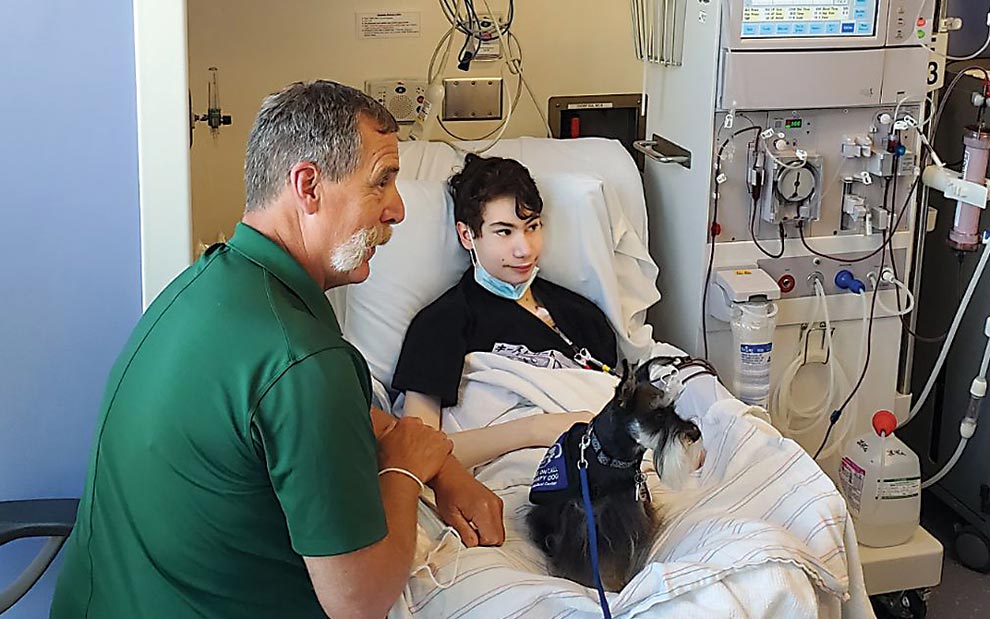
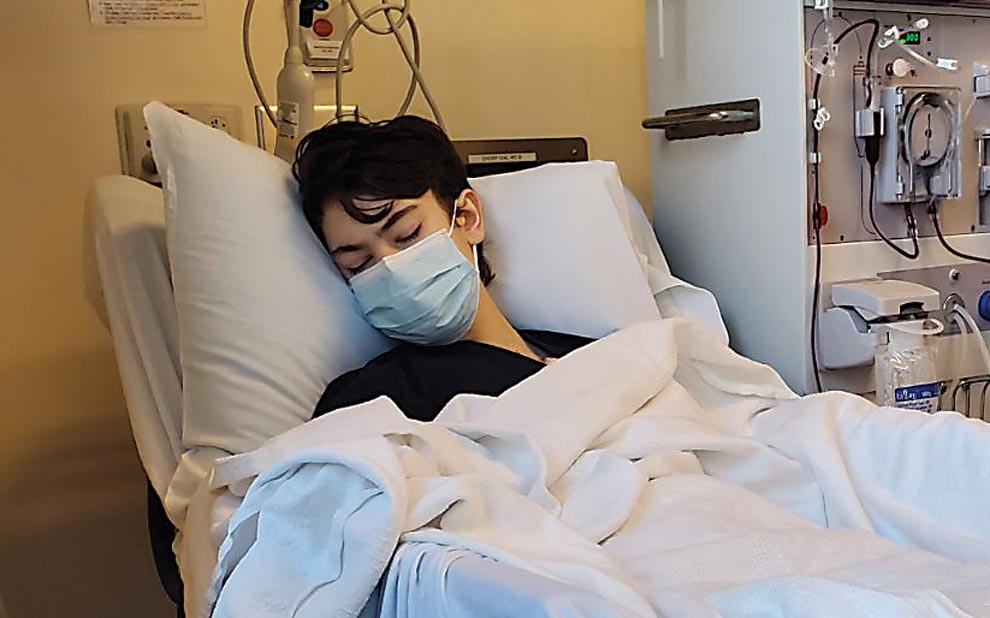
Delano’s kidneys were severely damaged. He had to start dialysis three days a week, which he says was exhausting. Delano was grateful for the procedure that was keeping him alive, but the whole experience took a toll, both mentally and physically. “To sit there for three hours knowing this [was] saving my life and knowing this [was] the thing that was keeping me alive … it was so mentally frustrating,” says Delano.
Unfortunately, after months of this process and two biopsies to check his kidney status, he wasn’t bouncing back. “Delano has always been a healthy child,” says Jessica. “He had never even had strep throat or an ear infection before, but when he went into the hospital, he only had five percent usage of his kidneys.” The granulomatosis with polyangiitis had left its mark. “There was no recovery from this with just the dialysis.” Finally, the medical team determined that a kidney transplant was the solution. Delano was placed on the transplant list in December of 2021.

When a Transplant Is Needed: Matching Kids with Organs
Doctors at CHoR advised the Dulins that the process for finding a kidney for Delano could take a year or longer. Jessica and Jonathan, Delano’s father, describe the waiting as excruciating. Delano’s type O blood might also impact the donor match. As the universal donor blood, type O blood can go to any other type; however, a recipient like Delano with type O blood must have a type O donor. During this time, the family was amazed by the number of friends, family members, and even strangers who volunteered to be tested to serve as a potential donor. No match was found.
After only six weeks on the waiting list, the Dulin family received fantastic news – a match had been found. Delano was already a patient at CHoR, one of four pediatric transplant programs in Virginia and 106 across the country. The kidney transplant surgery was scheduled for mid-January 2022.
Timothy Bunchman, MD, led the team that would perform Delano’s surgery. As professor and chief of the Division of Pediatric Nephrology, Dr. Bunchman manages the nephrology program at CHoR with a team approach, addressing everything from nutrition to disease education and more, ensuring patients and their families are at the center of every decision.
According to Dr. Bunchman, the transplant team completes around twelve transplants a year. Most hospitals only complete about three a year. Dr. Bunchman, who is responsible for selecting kidneys for the children his team treats, says he is highly particular when it comes to the process. “I turn down a lot of kidneys for children,” says Dr. Bunchman. “I want to put a really good kidney in a child.”
The pediatric team at CHoR consists of transplant surgeons, nurses, specialists, as well as a dietitian, a pharmacist, and a social worker. Prior to the surgery, an institution-wide meeting is held where the patient and surgery are evaluated. Once the team is given the green light, the surgery can be scheduled.
Delano’s Gift of Life
Delano’s transplant kidney came from a non-living donor, a gift for which his family will forever be grateful. Today, about half of all kidney donations come from living donors and half come from non-living donors. The kidney transplant surgery is a relatively short process, taking approximately four hours. Delano’s kidney was a match, and as his dad says, “it took to his body right away.”
Jonathan adds that it was evident from day one that the match was successful. “Normally, they have to jump-start the kidney and start dialysis, but as soon as they put it in [Delano] and plugged everything up, it was a 100 percent match and he got his color back!”
According to Dr. Bunchman, the recovery process for children seems to go more smoothly than it does for most adults. “It depends on the health and stability of the child going into the operating room. School-age kids and teenage kids sometimes need a little bit of oxygen and pain medication, and next they are up and walking and after five or six days, they are going home,” says Dr. Bunchman.
Delano’s mom Jessica says her son was not the typical teen when it came to recovery. “Delano was up the next day!” she says. “He spent two days in ICU and three days on the main floor and thankfully, he didn’t take any painkillers.”
After the successful surgery, Jessica was also able to get some rest. “When we knew he was finally safe,” says Jessica, “I crashed and rested, and [Johnathan] spent more nights with him in the hospital.”
Dr. Bunchman says the in-hospital recovery period for kidney transplant surgery has decreased rapidly due to the quality of medication and the surgical techniques. Once the child goes home, recovery continues. Most children have somewhere between fifteen to twenty-five doses of medications. These medications include anti-rejection and anti-viral agents. By about six months, it goes down to a six-medication list.
Kidney transplant recipients will remain on a life-long immunosuppressant. Dr. Bunchman says that can be hard for children to manage, and families receive lots of guidance on compliance to ensure long-term health. “It would be a disaster on so many levels if a seventeen-year-old lost a transplanted kidney due to not staying on their medication,” says Dr. Bunchman.
Life After Kidney Transplant Surgery
While it took a while to get adjusted to all of the medications, Delano has not had any problems adjusting to his new kidney. He visits CHoR every few months for check-ups but is carrying on with his life as a now sixteen-year-old. Delano loves art and enjoys playing the bass guitar, something he learned to do while he was home recovering. “I had always been interested in the bass and then got on dialysis and was isolated and really started playing it.” His main goal for now, though, is to “simply stay out of the hospital,” he says.
The family remains forever indebted to Dr. Bunchman and the entire team at CHoR. “Dr. Bunchman is one of the most playful, direct, and caring people you will ever meet. He is amazing. He has been so good to us,” Jessica says, noting that the doctor and her son developed a special relationship.
The Dulins agree the entire care team went above and beyond during the entire process – from diagnosing Delano to sending him home with a new kidney. “Doctor Bunchman, the nurses, the dialysis team – we became like a family. They were such a huge support system for everyone. When he was down and depressed and scared to death, the care team gathered around us.”
The Dulins also were fortunate to take advantage of the Ronald McDonald House while Delano was receiving care. “We were lucky enough to be able to travel back and forth [from the family home in Richmond County], but for the families who can’t, [RMHC] will put you up in a residence and provide you with meals and entertainment,” says Jessica.

Support from a Caring Community
Delano learned a lot from this life-changing ordeal. He attributes the support of his family to helping him make it through. His older sister Sierra provided counsel during some of his lowest times. “Make sure you are communicating to people,” says Delano about surviving a serious health challenge as a teen. “Be honest and open about it. If you don’t talk about it, you can go to dark places.”
The family is grateful to the members of the community who rallied around them during the crisis. Jonathan remembers during the 2021 holiday season, his company, Kaeser Compressors, gave the family a small battery-operated Christmas tree decorated with gift cards. “People we had never even met before were reaching out.” A GoFundMe account was created to help the family with their travel expenses. When the call for a kidney went out, a coworker of Jonathan’s was tested, and although she wasn’t a match for Delano, she ended up being a match for someone else and donated her kidney anyway.
Jessica also learned a valuable lesson about the kindness of others during this time. “People we don’t even know were donating [to help us]. Before my son got sick, I didn’t have the greatest faith in people. Then I saw how many people truly care about other people,” Jessica says. “That’s my lesson: People truly do care. Don’t be so quick to shut them down when they offer their help. It’s been overwhelming and it’s a lesson that I have learned, and I have truly taken to heart.”
A year and a half later, Delano is pretty much back to living the life of a normal teenager with his new kidney. During his health ordeal, he was selected as a Make-A-Wish recipient. His wish? A new bass guitar which he should be receiving in a few months.
For other kids and teens who find themselves in a situation like this, Delano shares this insight: “Never ever knock yourself down and think that nothing is going to get better for you. You just have to build up the courage that it’s going to happen. Life is always going to get better – no matter how dark or negative,” says Delano. “There will always be a light at the end of the tunnel and never doubt yourself for thinking that.”
Dr. Bunchman credits UNOS, the Richmond-based private nonprofit organization that manages the nation’s organ transplant system. “UNOS is really important because it oversees the equity and the ethics of organ transplants. It makes it so that everyone gets the same access to the [organ] donations,” says Dr. Bunchman.
The Dulins plan to acknowledge the donor and the gift of life that was given to Delano. “We want to give the donor’s family more time, but we are anxious to reach out. I want to write a love letter to thank them,” says Jessica. “We definitely would love to shout that family’s name from the mountain tops.”

Tribute to Andrew: The Gift of Life
When my nephew Andrew passed away at the age of eleven last year, my family suffered a loss from which we will never fully recover. The youngest of four, my sister calls Andrew her “beautiful surprise baby.” He loved baseball, guacamole, and animals.
He will be forever missed, but four of Andrew’s organs – both kidneys, his heart, and his liver – were transplanted to help four other young people who live with life-altering health challenges.
Andrew’s parents, Shiree and Eric Parnell, are grateful to the staff at Children’s Hospital of Richmond at VCU and Donate Life Virginia for helping them understand the good that can come from a tragic situation.
“Donating [Andrew’s organs] allowed us to spend more time with Andrew in the hospital than if we hadn’t donated,” says Shiree, who explained that Andrew was kept alive for three additional days while health care providers and UNOS representatives worked to evaluate his organs and find potential matches.
Shiree said the staff at CHoR helped them celebrate Andrew’s life in a truly memorable way. “The honor walk that was held for him as he [was transported] to his donation surgery made us feel as if he was a true superhero,” says Shiree. “The entire hospital wing lined up to honor him.”
Throughout this past year, Donate Life has continued to uplift my sister and her family by hosting donor family events that allow them to connect with donor and recipient families from all over the region. These events will continue to help them see the true impact of their son’s donations on other families’ lives. If you want to learn more about organ donation, visit DonateLifeVirginia.org.





